Estonia Comes To Aid Of HIV-positive Ukraine Refugees
When Svitlana fled war-torn Ukraine for Estonia, she not only had to contend with all the usual challenges of being a refugee, she also had her HIV treatment to worry about.
The 45-year-old, whose husband unknowingly infected her when they met, had been managing her illness for years with medication and now, in a new country, needed to ensure her supply.
“I was running out of pills… I tried to register for a doctor’s appointment on my own, but the waiting list was really long,” the mother-of-three told AFP.
Fortunately, at the refugee centre she came across information about the Estonian Network of People Living with HIV (EHPV), an NGO offering assistance.
Svitlana had come to the right place.
The organisation is well-versed in the ins and outs of the illness, having been around for nearly two decades as the country fought to rein in its transmission rate.
“I called the volunteer and told them about my problem… A few days passed and they got me a doctor’s appointment (and) went there with me.
“Right now, I’m on therapy I got in Estonia. I feel good, my test results are really good… My immunity is good and the viral load is zero,” she said.
“I’m not dangerous for society, other people. Neither in everyday life nor at work, anywhere.”
The spread of HIV was once out of control in Estonia.
For years the small Baltic state had the highest transmission rate within the European Union.
“We had a very difficult situation, a concentrated epidemic among injecting drug users,” said Lachin Aliyev, EHPV board chairman.
“But in 20 years we’ve been able to stabilise the situation,” Aliyev told AFP.
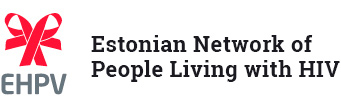
Things were at their worst at the turn of the century, with 1,474 new cases diagnosed in Estonia in 2001, or a rate of nearly 108 per 100,000 people.
Those figures have been falling steadily ever since, with 125 new cases and a rate of 9.4 reported in 2021, according to government data.
It was still one of the worst rates in the EU — surpassed only by those of Latvia and Cyprus, according to the World Health Organization — but it had improved.
“We’ve been working towards zero new cases of HIV, zero stigmatisation, no children born with HIV,” Aliyev said.
“But first there was Covid… and then the war started.”
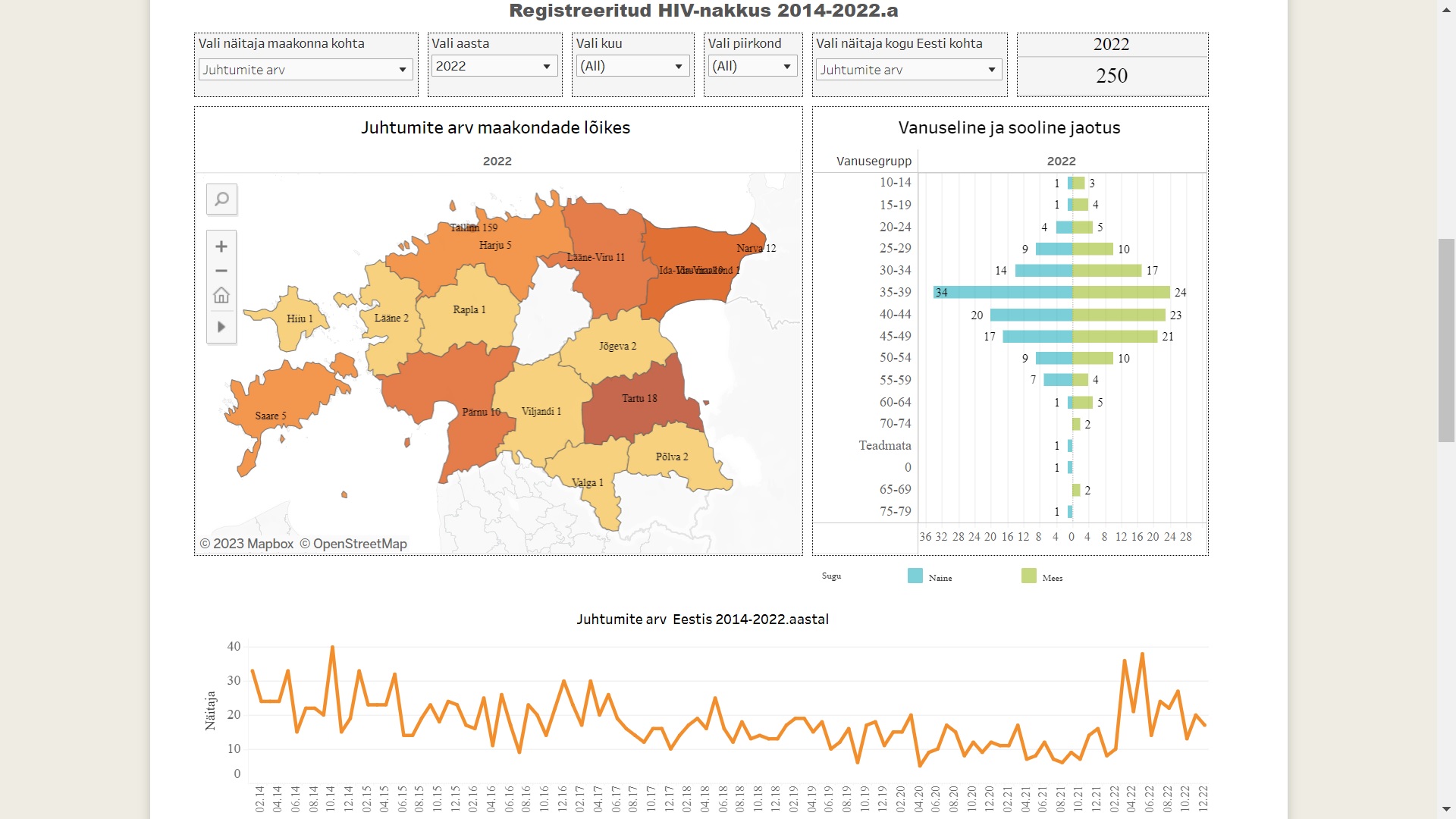
Since Russia’s invasion of Ukraine last year, tens of thousands of refugees have wound up in Estonia. Of those, a tiny percentage are HIV-positive.
There are currently just over 100 of them registered and receiving therapy in Estonia, according to health authorities.
Most had already been receiving treatment in Ukraine and it was crucial that they not run out of pills.
“Once it’s begun, the person shouldn’t stop treatment even for a day,” Aliyev said.
“Medication must be available, so that the person doesn’t develop resistance if they suddenly stop taking them,” he added.
In addition to helping the refugees with any medical issues, EHPV offers a support group where they can vent and problem-solve in Ukrainian.
The organisation also fights stigma, as the slight uptick in new cases, including in regions that had virtually none, has led to disinformation and fear-mongering against refugees.
“It has frightened people a bit, and politicians have encouraged this fear and started manipulating it,” Aliyev said.
“Our task is to explain that people receiving treatment have zero viral load, there is no virus in their blood and they don’t spread it,” he added.
https://www.barrons.com/articles/estonia-comes-to-aid-of-hiv-positive-ukraine-refugees-01674282310




































 Despite the fact that the immunodeficiency virus is the most studied virus on the planet, most people still do not have clear understanding of what HIV is.
Despite the fact that the immunodeficiency virus is the most studied virus on the planet, most people still do not have clear understanding of what HIV is.
